Challenge in Bihar
In the tumultuous arena of Bihar politics, where alliances shift like sand dunes in the wind, this election seems poised to redefine the political landscape.
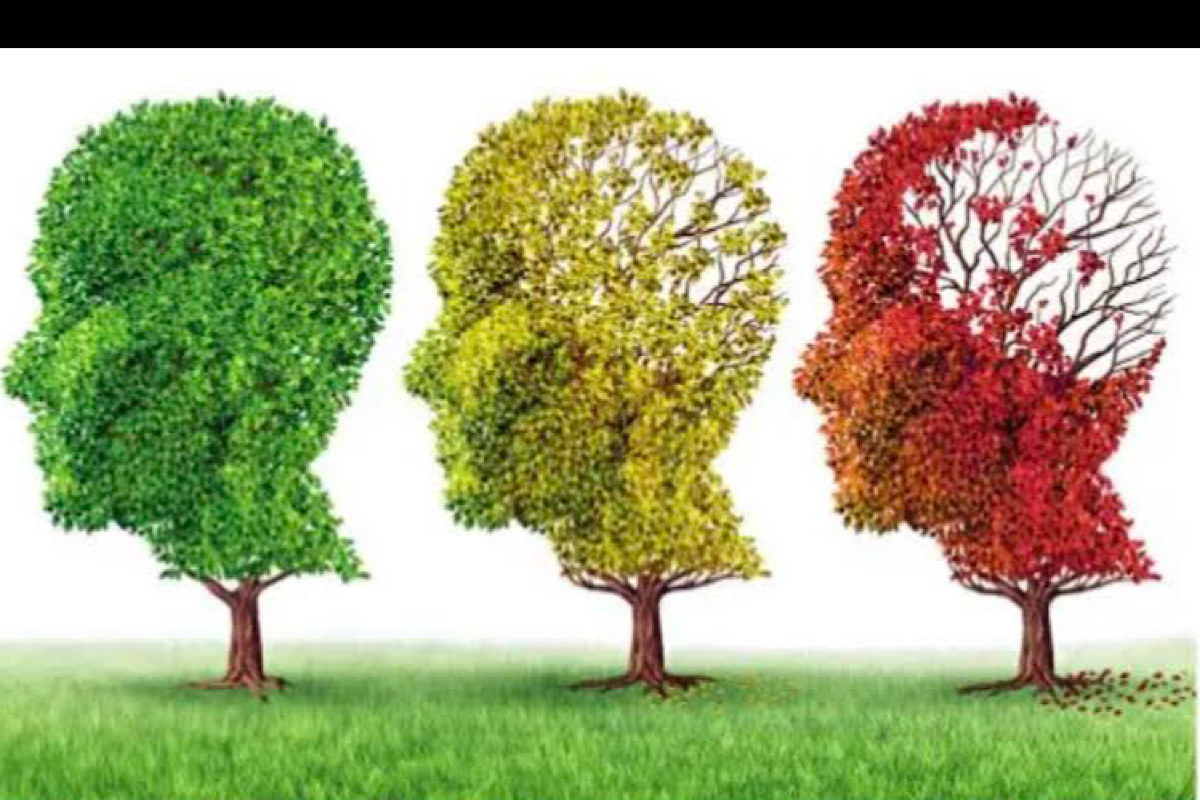
Representation image
2 1st September is World Alzheimer’s Day; the theme this year is Never Too Early; Never Too Late (to diagnose and manage). Dementia is a common illness that affects elderly people and its prevalence is on the rise, with increasing longevity. More than 55 million people are estimated to live with dementia worldwide, as per 2020 data. One new case is diagnosed every three seconds. As per Dementia India 2020 report, there are about 53 lakh people with dementia in India, with estimated rates of 5-7 per cent of the elderly population. This number is increasing day by day with the exponential rise of the elderly population.
This is going to challenge the country’s health care system. The disorder is common in females, which could be because of their relatively longer life span. It affects the rich or poor and those living in urban or rural dwellers. Dementia is an umbrella term, and there are many types, of which Alzheimer’s disease is the commonest. There is an abnormality in the amyloid protein of the nerve cell membrane that gets broken at the wrong position and becomes sticky and insoluble, clumps together, and gets deposited in between nerve cells, termed as amyloid plaques, which unusually cannot be expelled from the body. These plaques are toxic causing breaks in the nerve cell connections and also lead to nerve cell death.
There is another protein inside the cells which is meant to be the skeleton of the cell. This becomes abnormal, leading to falling off the skeleton, leading to nerve cell death. Such cell deaths keep occurring gradually in different areas of the brain, hampering the pertinent function of that brain area.
Advertisement
The next common type is Vascular Dementia which can also be considered as multiple mini-strokes occurring in the brain, leading to a shortage of blood supply, which in turn means a lesser supply of oxygen and glucose leading to nerve cell damage or death.
There are Lewy body and Parkinson’s types of dementia, which are due to an abnormality in a protein called alpha-synuclein that misfolds and becomes toxic leading to death or degeneration of nerve cells. Another type of dementia which is common and starts a bit early in life, may be in the sixth decade itself for many, is called Frontotemporal dementia, which is again due to irreversible abnormal protein deposition leading to degeneration. For discussion here, Alzheimer’s disease type is taken as an example. There is a gradual decline in mental functions such as memory, attention, thinking, reasoning, ability to navigate, planning, decision-making, judgement, and calculation. Higher skill-based functioning such as cooking or financial transactions may be first to go followed by impairment in the basic ones such as the ability to take a bath, brush, comb hair, dress, and groom.
Family members can notice a gradual downward trend in their level of functioning in comparison with their previous functioning. The illness severity increases over time leading to dependency on caregiving relatives, usually elderly spouses or children. Typical Alzheimer’s disease starts with forgetfulness for recent events or experiences with intact longer-term memory. Gradually it worsens over about five years on average and the person may lose the ability to walk, talk, not able to identify family, and require complete care. It is never too early to diagnose dementia.
The earlier it is done, the better. The psychiatrists or neurologists gather detailed information from a relative about how it started, and the presenting problems, and do memory tests, blood tests, and brain scans. One of the aims of this assessment would be to find out if it is a reversible condition. This includes depression, deficiency of vitamin B12, low thyroid, autoimmune illnesses, confusion due to infection of the urinary system or the chest, and any abnormal growth inside the brain. Many of these conditions are treatable and therefore should be ruled out first.
Detecting dementia early helps in planning their years, and anticipating the increasing care needs. A person with early signs of dementia can choose to nominate any of the relatives to decide for them about care or any other social aspects.
They can consider doing a ‘will’ when they understand the concept of a ‘will’ and about their finances while having the decision-making ability. The person must get involved in stimulating activities, such as increasing social interaction, doing problem-solving activities, solving puzzles, and if interested can do sudoku kind of activities.
The DEMCARES team in Chennai in collaboration with a team in London, have developed cognitive stimulation therapy which has modules of activities in group and on individual basis. Similarly, a few mobile apps enhance stimulation or a kind of retraining to the brain and some more are being developed. It is never too late to diagnose dementia. Unfortunately, there is no complete cure as of now, so the condition cannot be reversed, which means a person with dementia will not regain the lost skills.
Education and training to caregiving family members as to how to interact, what to do, and what to expect will reduce their distress, and enhance their ability to care. One could discuss with their treating clinician regarding any social schemes to support patients and their caregivers. Regular activities to keep them engaged in group or at individual level is important, but difficulties may be due to lack of time from the family caregivers. Restlessness comes down with regular structured activities that occupy the mind.
Caregivers’ support network to try to find practical solutions from one another has been found useful. Caregivers need to take regular breaks from this routine of caring, as characteristically, with the disease getting worse, care needs become more demanding. The role of paid, formal, professional caregivers cannot be underestimated. They stay with the person, ensure personal care, grooming and timely medications, and engage in activities aimed at comfort, while managing basic care and safety.
Caregiving is an art and requires people equipped with caring and communication skills. This reduces the stress on the family members. Training and supervision of such dedicated caregivers helps improve quality of life and maintain comfort. This will prevent the need for residential care facilities, and increase the chance of care at home. Disease-reversing medications or the antibody kind of treatment aimed to remove plaques and tau deposits are under progress with not much success as of yet, though a couple of medications have received conditional approval for use in the USA.
Medications to reduce the speed of worsening are regularly being used. Caregiver distress increases due to the behavioral problems of the person such as aggression or restlessness. Instead of straightaway considering medications to calm them down, there is a need to try to identify the source of these behaviors. This may be due to tooth infection, pain anywhere in the body, constipation, overstimulation, fear due to abnormal experiences, and low sugar levels.
Those wanting to try and prevent or delay the condition can work on the risk factors by improving their lifestyle. Controlling blood pressure, maintaining blood sugar levels, reducing overweight, and avoiding smoking will reduce the risk. Depression must be identified early and treated. Avoid a sedentary lifestyle, and engage in meaningful, pleasurable activities. Increase social interaction by spending time with family and friends. Yoga, meditation, and reducing stress due to work, or social problems may all help indirectly. Management of dementia requires a multi-specialty approach.
There is a need for nursing, speech, and language training, to improve hearing, improve vision, and ensure safety at home with help from occupational therapists. There is a need to improve community-level care by training primary care physicians and ASHA workers to identify cases early.
There is a need to increase the number of specialists who can lead the care plan. The geriatric psychiatry team at NIMHANS has provided certified training to over 200 professional caregivers and over 100 general practitioners or specialist physicians. Volunteer training is also underway, and there is a need for community sensitization. Incentives for family caregivers reduce the burden on the public health care system.
(The writer is on the Geriatric Psychiatry Faculty at NIMHANS, Bangalore)
Advertisement