Yoga: An escape from monotony to a healthier lifestyle
Mind-body interventions such as yoga and meditation have been proven to have a pronounced and radical impact on our physical and mental health.
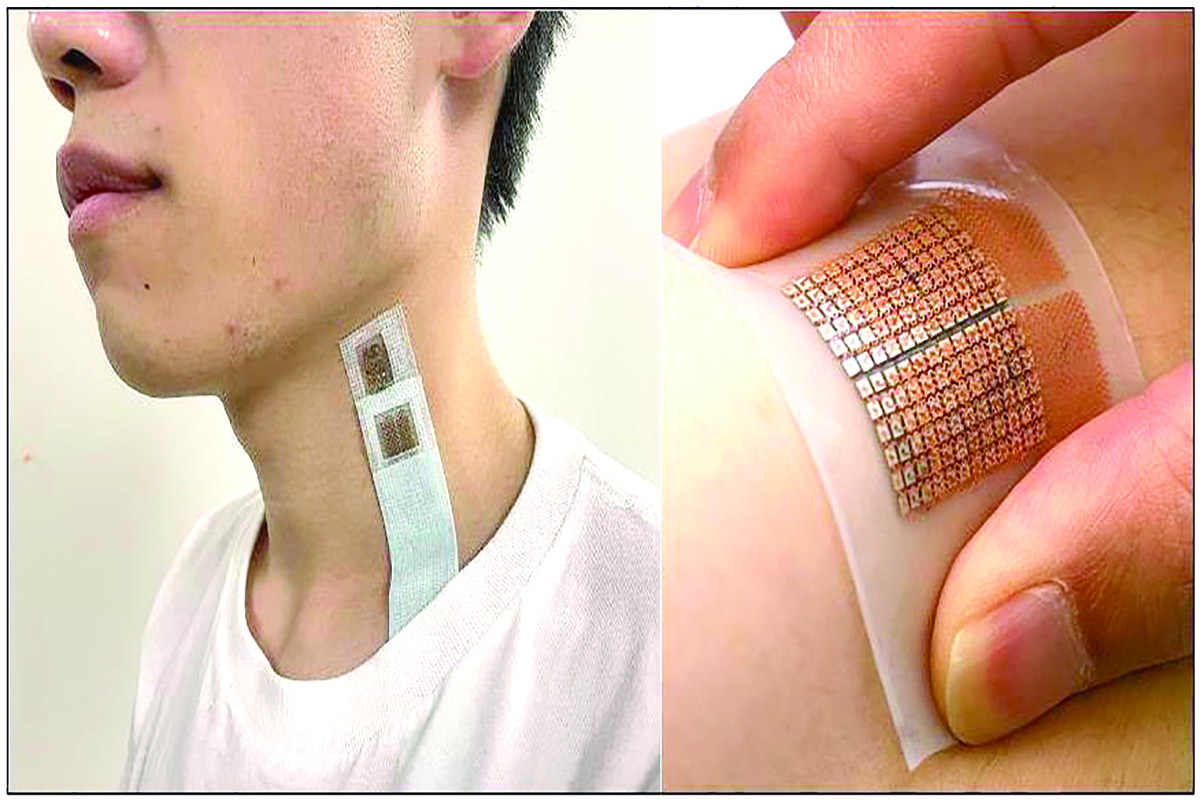
A prototype wearable skin patch uses sound waves to provide good quality, real-time images of internal organs
The organs of the body, which a doctor treats, are invisible. Till not so long ago, diagnoses were based only on signs that could be made out on the surface. But now, a doctor has lab reports, x-ray pictures and scan reports to help her.
The x-ray was the first probe that provided physicians a picture, without the need for surgery, of the state of tissues within the body. X-rays are a form of light, but of short wavelength, which enables them to pass through soft tissue.
Many decades later, sound waves, which were used to detect flaws in things made of metal, found an application in medicine. The wavelength, again, was shorter than of audible sound, to be of dimensions close to those of the things to be imaged. Then entered electronics and computers. The computed tomography, or CT scan, was a series of X-ray pictures that were taken in slices through parts of the body and put together to create 3-D images. And ultrasound scans, with a probe that directed ultrasound into the body and displayed images on a computer screen, with the facility for measurements and recording the images — this was the ultrasound sonograph, or USG.
Further tools that became available were magnetic resonance imaging, or MRI, which scanned the response of substances in cells to wireless radiation and strong magnetic fields, and positron emission tomography scan or PET, which works with radioactive tracers. Such advances have extended the range of information that medical persons have to diagnose, plan treatment and monitor results. The drawback, however, is that the scans need large pieces of equipment, take some time, and are expensive. A paper in the journal, Nature, Biomedical Engineering, now reports a development in stark contrast — a wearable skin patch, just a few centimetres across, which uses sound waves to provide good quality, real-time images of internal organs, and for as long as the wearer carries the patch. Chonghe Wang, Baiyan Qi, Muyang Lin, Zhuorui Zhang, Mitsutoshi Makihata, Boyu Liu, Sai Zhou, Yi-hsi Huang, Hongjie Hu, Yue Gu, Yimu Chen, Yusheng Lei, Taeyoon Lee, Shu Chien, Kyung-In Jang, Erik B Kistler and Sheng Xu , from the University of California, San Diego, Harvard University, Yonsei University, Korea Institute of Science and Technology, Seoul, Daegu Dyeongbuk Institute of Science and Technology, Daegu, Republic of Korea, describe a prototype of the skin patch, which can focus upon and monitor the dynamics of blood flow from as deep as 14 cm inside the body.
“Most chronic diseases directly manifest on one or more deep tissues. Thus, continuous and non-invasive monitoring of physiological signals in deep tissues to interrogate disease initiation and progression is paramount to support clinical decisions for diagnosing and treating chronic diseases,” the paper says. Now, what it calls for is something that can penetrate the tissue surrounding the organ of interest and carry back useful information without being cumbersome. Advances in communications and electronics have created possibilities of miniaturisation and portability. The information from a hand-held USG probe can connect to a cell phone, dispensing with the need of larger equipment, or permit the scan to be performed over a telecom link. The drawback, however, is that it cannot be continuous or done without a technician. The answer, the paper says, appears to lie in stretchable electronics — devices that could be attached to a patient’s body, monitoring her medical condition continuously, while she goes about her work, and not only at a specialised clinic. The devices would include electronic circuits to drive generators and detectors of different kinds of waves, devices to convert the reflection into electrical records, arrangements to record and transmit the information, the power supply, etc. The devices need to be embedded in a flexible substrate, like silicone or polyurethane. And the interconnections must have the slack that allows the substrate to bend or use conductors that are stretchable. These conditions have been approximated, but optical or other electromagnetic waves, even chemical or heat signals, in the probe, do not have the ability, either to reach the target organs, or if it were possible, to usefully resolve an image, the paper says. High frequency sound waves, however, do have the capacity to penetrate human tissue and with electronics, we can arrange for a panel of sources, which create a focused and directed beam of sound waves to select tissue masses of interest. A single source of waves would spread out, like the ripples on a pond and grow rapidly weaker. If there were a pair of sources, however, there would be a plane, between the sources, where the waves would add, and become stronger. And with more sources, the region where the waves from all the sources add could be arranged to be a narrow beam, or a small volume, and the waves in the region would be powerful. With the control of the timing from different sources, called the “phased array technique”, the region of concentrated waves could be moved and adjusted. “An unfocused single element has a penetration depth of three to four cm and can sense a region directly beneath it. Considering the complexity of human anatomy, it is very challenging to target specific regions with a single element. The phased array technique, which synchronises an array of transducers to enhance the energy density and enable beam steering, is ideal for overcoming this challenge,” the paper says. The team has hence developed a panel of 12 millimetre-sized ultrasound generators, a number that can be increased to 128, embedded in a flexible, polymer medium. The interconnections are with “serpentine” wires, so that the device can be bent or stretched. And each device is separately controlled by a computer, which, conceivably, could be in a microchip, embedded in the device.
The flexible strip containing the device could be attached to the body, say the chest or neck, and it would follow the contours of the body if the wearer stretches or bends. As ultrasound is absorbed by air, it is important to avoid air gaps between the source and skin of the wearer. That is the reason for the special gel when a hand-held device is used to probe the body for the usual USG scan. With the flexible strip, however, close contact with body contours eliminates the need for a gel, and the strip can be in place for extended periods.
“The device allows for active focusing and steering of ultrasound beams over a range of incident angles so as to target regions of interest,” the paper says. For the best convergence of the ultrasound beam, the wavelength needs to be near the spacing of the elements in the phased array. And then, a longer wavelength is good for deep penetration, but not for image resolution. The authors therefore selected a wavelength that best satisfied the conflicting requirements. In a proof of concept, the authors probe the left and right ventricles of the human heart and record the blood flow, by measuring the “Doppler effect” — the effect that the movement of blood has on the frequency of the reflected sound waves. “The ultrasonic beam could be steered to intercept blood flow at an appropriate Doppler angle, allowing accurate recordings of blood flow spectra in major arteries and veins. Combining the blood flow and vessel dimension measurements, we were able to estimate cerebral blood flow in real time,” they say. The device could be coupled with an intelligent unit the wearer could carry, one that would record relevant body parameters over hours or days, possibly communicate with a medical team and even raise an alarm when specific features are seen.
Advertisement
Advertisement